:max_bytes(150000):strip_icc()/pulsus-paradoxus-4587588-v1-593d02d7f4ab4380894939e7ce04c44d.png) Understanding the Mechanism of Pulsus Paradoxus
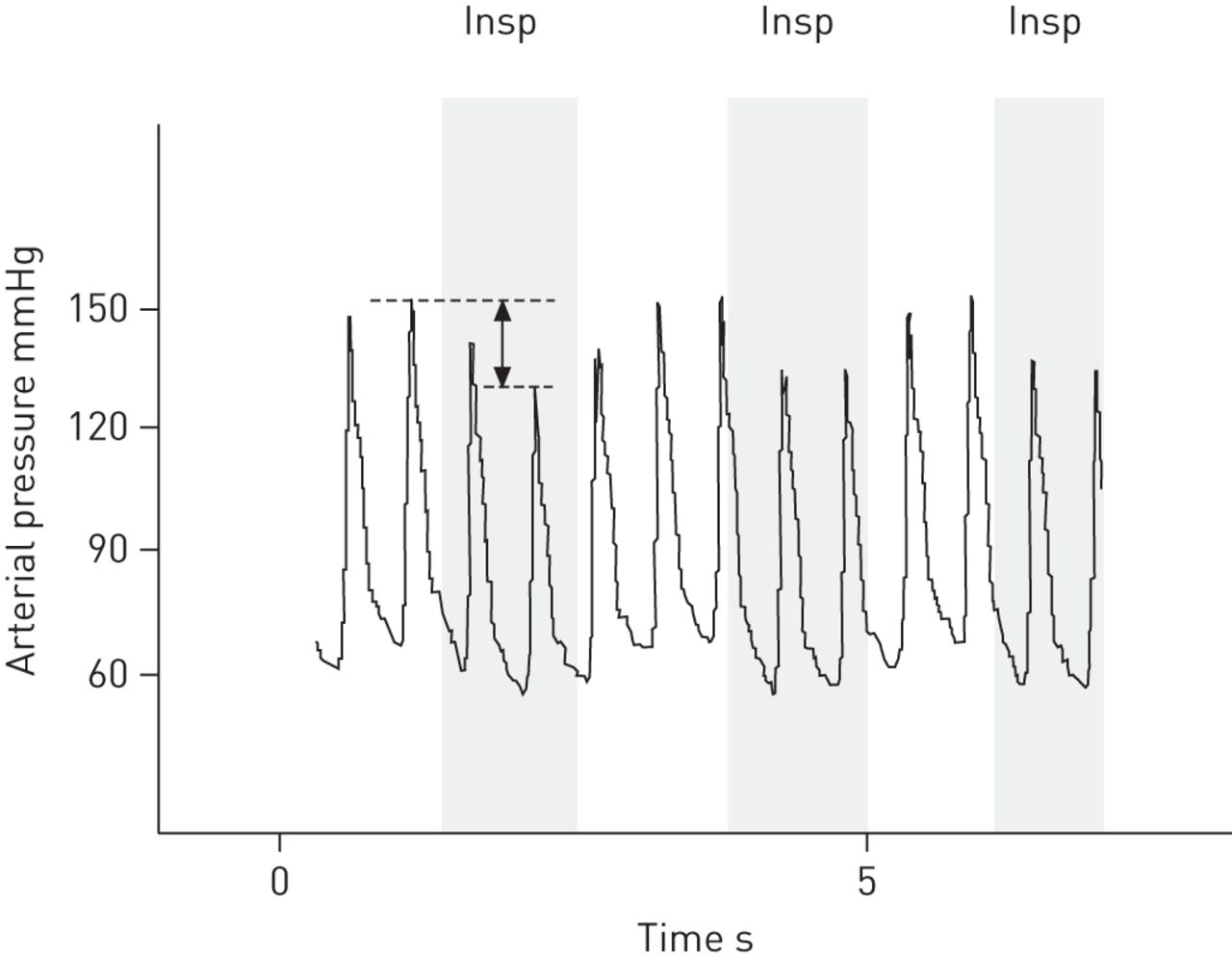
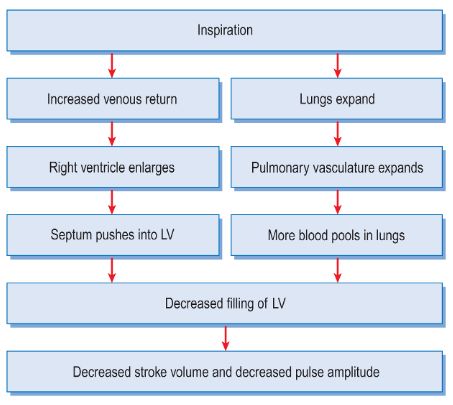
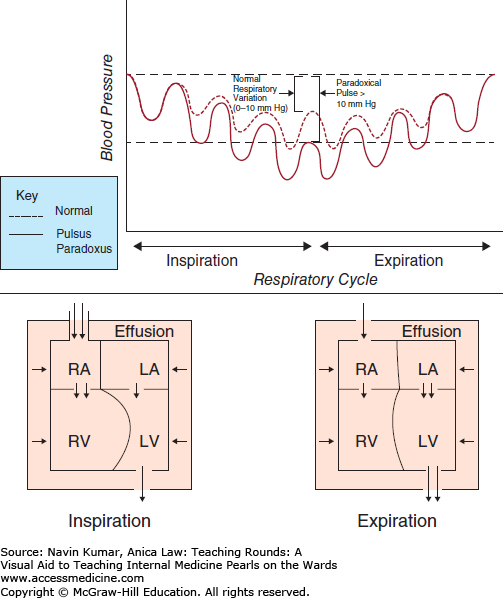
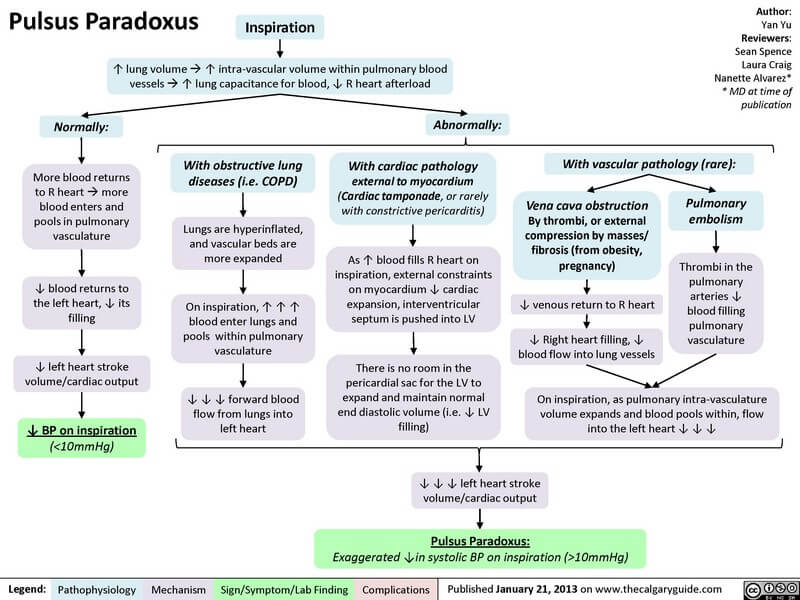
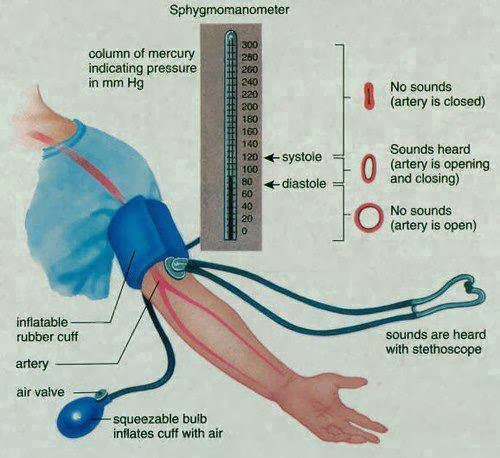
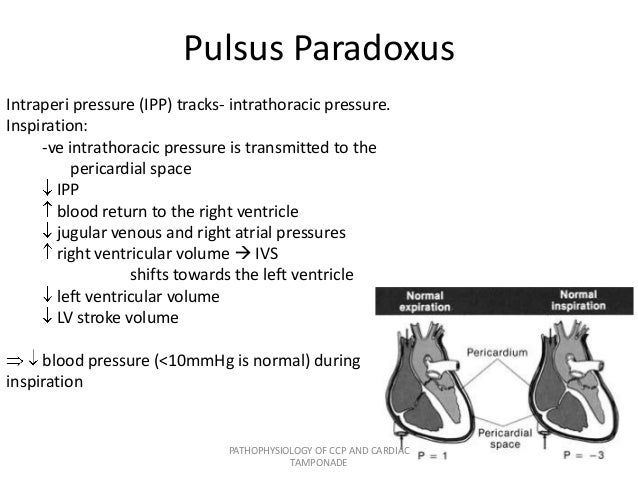
Understanding the Mechanism of Pulsus ParadoxusWarning: The NCBI website requires JavaScript to operate. NCBI Bookshelf. Service of the National Library of Medicine, National Institutes of Health. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan... StatPearls [Internet]. Pulsus Paradoxus Matthew N. Van Dam; Brian M. Fitzgerald.AuthorsAfiliations Last updated: November 19, 2020. Continuous educational activityPulsus paradoxus refers to a systolic pressure drop of more than 10mmHg during inspiration. Pulse paradoxus is due to alterations of mechanical forces imposed on the chambers of the heart and pulmonary vasculature, and is often due to pericardial disease, in particular cardiac tamponada and a narrower degree constrictive pericarditis. However, it is important to recognize that paradox pulsus can be seen in non-pericardial heart diseases such as the right myocardial infarction and restrictive myocardiopathy. In addition, non-cardiovascular conditions, including lung diseases such as severe chronic obstructive pulmonary disease, asthma, tension pneumothorax, large bilateral pleural effusion and pulmonary embolism can lead to pulse paradox. Other causes include any condition that results in heart compression, such as iatrogenic compression during surgery, marked obesity and excavatum pectus. Finally, the pulpsus paradoxus can also manifest hypovolemic shock secondary to severe. This activity describes the pathophysiology, evaluation and management of the pulpsus paradoxus and highlights the role of the interprofessional team in the care of patients with pulpsus paradoxus. Objectives:IntroductionPulsus paradoxus refers to an exaggerated drop in a patient's blood pressure during inspiration for more than 10 mm Hg. Pulsus paradoxus results from alterations in mechanical forces imposed on the chambers of the heart and pulmonary vasculature often due to pericardial disease, in particular the cardiac tamponate and a minor constrictive pericarditis. However, it is important to understand that paradox pulsus can be seen in non-pericardial heart diseases such as the right myocardial infarction and restrictive myocardiopathy. In addition, non-cardiovascular disease states may occasionally lead to pulsus paradoxus including lung disease (total chronic obstructive pulmonary disease [COPD], asthma, tension pneumothorax, large bilateral pleural strokes, pulmonary embolism), as well as any cause of heart compression (iatrogenic during surgery, marked obesity, excavatum pectus). Finally, the pulpsus paradoxus can also manifest hypovolemic shock secondary to severe. EtiologyAs mentioned above, paradox pulsus is typically manifested in patients with pericardial disease, in particular cardiac tamponate and constrictive pericarditis. Other heart causes include right ventricular infarction and restrictive myocardiopathy. In addition, non-Cardiovascular disease states can also lead to pulsus paradoxus including lung disease (with COPD, asthma, tension pneumothorax, large bilateral pleural efusions, pulmonary embolism), as well as any cause of heart compression (citrogenic during surgery, marked obesity, excavatum pectus). Epidemiology The epidemiology of the pulpsus paradoxus is difficult to define because of the heterogeneity of the diseases that lead to its manifestation. The incidence of cardiac tamponate leading to the pulsus paradox has been poorly documented. A retrospective study of a single center of 136 patients admitted to cardiac tamponate diagnosis, the main causes were malignancy (32%), infection (24%), idiopathic (16%), iatrogen (15%), postmiocardial infarction (7%), uremic (4 %), and other causes (2%). However, the number of people who developed paradox polishsus was not noted. Although the statistics relating to the pulsus paradox in the heart tamponate are limited, it is believed to occur in most cases. In a prospective study of 15 patients with cardiac tamponada, pulsus paradoxus was present in 10 of 15 patients (66.6%). Patophysiology To really understand the physiopathology of the pulpsus paradoxus, we must explore the normal respirophatic effects of chest mechanics on blood pressure. In healthy individuals, there are normal phase changes in the heart output that occur with breathing. During inspiration, there is a small decrease in systemic blood pressure of less than 10 mm Hg. Inhaling, intrapleural pressure decreases; there is a decrease in intrathoracic pressure that promotes venous entry into the chest by increasing the right heart filling. However, this does not amount to an increase in the filling of the left heart during inspiration. This is because, as one inhales, the lungs expand and pull radial traction over the pulmonary vasculature by increasing their capacitance, sequestering blood in the chest momentarily, and lowering blood flow to the left heart, decreasing pre-load and consequently the cardiac output. The opposite occurs during expiration, so systolic pressure usually decreases during inspiration and increases during expiration. So why does the term pulsus paradoxus imply the drop of blood pressure during inspiration is paradoxical? The term pulsus paradoxus was coined by German physician Adolph Kussmaul who referred to the palpated pulse of affected patients being of variable force despite the regular precordial activity. The physiopathology of the pulpsus paradoxus is complex and varies depending on etiology; there are several mechanisms involved. In the heart tamponate that results in paradox pulsus, the physiological fall of the cardiac output is exaggerated for several reasons; however, the most significant is the enhanced ventricular chamber interaction, often called ventricular interdependence. Increased pericardial pressure limits the ability of the right ventricular free wall to expand and accommodate the flow of blood during inspiration. The result increases the ventricular septal tilt to the left ventricle, as the blood fills the right heart, which results in a lower diastolic volume of the left ventricular end, a lower traction volume and a lower systolic pressure. In simpler terms, in a non-compatible pericardial space, so that the right heart fills more inspiration, the left heart should fill less. As pericardic pressure increases, the compliance of the ventricles decreases until, under extreme pressure, the effective compliance of all the chambers meets that of pericardial space. In advanced tamponada, intrapericardial pressure will be the key factor in determining diastolic heart pressures. This is why a doctor will see an equalization of chamber pressures during the diastole in the heart tamponate. In constrictive pericarditis, a separate mechanism may be involved. During normal inspiration, intrapleural and intrapericardial pressure falls into tandem to about the same degree, and this pressure drop is transmitted to the heart chambers. In constrictive pericarditis, the thickened pericardio will prevent the normal decrease in the pressure from reaching the ventricles; therefore, the normal fall of the filling pressures will be swept by the thick pericide. This is important because in the pulmonary veins (which are extrapericardial), the fall of the pressure will be greater than the fall of the left ventricular diastolic pressure (intrapericardial), and the gradient will be reduced for the left ventricular filling, which will reduce the left ventricular filling. The opposite occurs during the expiration. Another mechanism to consider is the effect of inspiration on left ventricular transmural pressure. The left ventricular transmural pressure is the sum of intracavity pressure less the negative intratoric pressure generated during the inspiration. Since the left ventricle is contracted during inspiration, it must do so against negative intrathoracic pressure. This increases the stress of the left ventricular wall and the subsequent load and effectively decreases systolic aortic pressure. This mechanism is exaggerated in a severe lung disease that requires significant negative intrathoracic pressures during inspiration such as COPD, asthma and obstructive sleep apnea. History and paradox FisticoPulsus is a clinical test that can be seen in a variety of disease processes. It is a key test in pericardial effusion as it can herald of cardiac tamponada. In pericardial effusion, the presence of pulsus paradoxus has a greater sensitivity of 80% for tamponado, and strongly increases the likelihood that tamponade is present. However, the absence of pulsus paradoxus does not exclude a diagnosis of cardiac tamponate. If present, polished paradoxes can be an indication that hemodynamic collapse is imminent; therefore, all patients with suspicion of tamponado and paradox pulsus should be evaluated for urgent or emerging pericardial drainage. The disease states in which the heart tamponate SIN pulsus paradoxus can occur include the following: Pulsus paradoxus can be seen in constrictive pericarditis, although less frequently than that seen in tamponade. A notable exception is constrictive pericarditis with pericardium derrame (submersible-constrictive pericarditis) in which a severe pulsus paradox is likely to be seen. As noted above, there are many states of disease other than pericardial pathology that can lead to pulsus paradoxus. The most common of these is severe asthma or COPD. In these states of disease, negative intratoric pressure generated is greatly amplified compared to healthy individuals, sometimes about 40 mm Hg under atmospheric pressure. These broad pressure changes will increase left ventricular transmural pressure and effectively increase VV load. In addition, the pressure will be transmitted to the intratoric aorta and to the downstream vessels. This can manifest as a polish paradox. One important thing to take into account when considering the paradox pulsus while discerning between pericardial and non-pericardial disease is the following: the paradox pulsus in non-pericardial disease will generally manifest with a fall in systolic and diastolic pressures. This contrasts with the pericardial disease in which the drop is mainly found in systolic pressure, diastolic pressure is usually minimally affected, so the pressure of the pulse will be narrower. EvaluationMeasuring Pulsus Paradoxus Pulsus paradoxus For patients without uninhabitant arterial access, the pulsus paradoxus is better measured with a manual sphygmomanometer and stethoscope. Automatic blood pressure cuffs cannot accurately measure for the pulpsus paradox. The evaluation is made inflating the cuff until all Korotkoffs are absent, and then very slowly releasing the cuff pressure. The first hidden sounds will be heard only during the expiration, and this pressure must be noticed. Next, as the pressure of the cuff drops further, the pressure must be noticed when the sounds of Korotkoff are heard during inspiration and expiration. The variation between these 2 systolic pressures is what quantifies the pulsus paradox. The paradox of the severe pulpsic can be appreciated as a weakening or demise of the palpated pulse during inspiration. In certain circumstances, the pulpsus paradoxus can be seen with respirophosic variations in the patient's pulse oxide wave as well. An important advice when evaluating for the pulsus paradox is to ensure normal breathing of the tide volume in the patient. Do not instruct them to change their breathing pattern as the depth of breathing influences the magnitude of the pulpsus paradoxus and will be amplified in patients with lung disease. For patients with abode arterial access, measuring the pulse paradox is as simple as observing the waveform and noting the difference in systolic pressure during the respiratory cycle. Because the drop in blood pressure is secondary to a drop in the left ventricular traction volume, the change in pressure observed during the paradox pulsus will mainly reflect a decrease in systolic pressure and pulse; diastolic pressure is usually minimally affected. The additional assessment of patients with pulsus paradox will depend on etiology. Importantly, if pericardial effusion is known or suspected, a diagnosis of cardiac tamponate should be considered, and an ECG, chest X-ray and transthoracic echocardiography should be obtained in the absence of hemodynamic involvement. If hemodynamic instability is present, the emerging drainage of the pericardial fluid should be considered. Treatment / ManagementPulsus paradoxus is not a condition of disease. It is a physiological manifestation of an underlying disease process and treatment should address the underlying pathology. If it is suspected that the heart tamponate and the pulsus paradox is present, urgent or emerging pericardiocentesis should be taken into account. An exception to this would be pericardial effusion secondary to aortic dissection or myocardial rupture; these patients require emergency surgical intervention. Differential Diagnosis Results of the Pulsus Paradoxus Health Team are best managed by an interprofessional team including nurses. Pulse paradox is not a condition of disease. It is a physiological manifestation of an underlying disease process and treatment should address the underlying pathology. If it is suspected that the heart tamponate and the pulsus paradox is present, urgent or emerging pericardiocentesis should be taken into account. Continuous Education / Review QuestionsReferences This book is distributed under the terms of the Creative Commons 4.0 International License, which allows the use, duplication, adaptation, distribution and reproduction in any medium or format, provided that you give appropriate credit to the original author(s) and source, a link to the Creative Commons license is provided, and the changes made are indicated. ViewsIn this PageRelated information Similar products in PubMed Recent activityYour navigation activity is empty. The activity recording is off. , 8600 Rockville Pike, Bethesda MD, 20894 USA
Pulse paradox Pulse paradoxus Pulse paradoxus, also paradoxic pulse or paradoxic pulse, is an abnormally large decrease in the stroke volume, and wave during . The normal pressure drop is less than 10 . When the drop is more than 10 mmHg, it is called polish paradox. Pulse paradox is not related to heart rate or pulse, and it is not a paradox increase of systolic pressure. The normal variation of blood pressure during breathing/breathing is a decrease in blood pressure during inhalation and an increase during exhalation. Pulsus paradoxus is an indicative of several conditions, including , chronic , and (for example , ). Pulso paradoxusparadoxic pulseparadox The paradox in pulsus paradoxus is that, in , you can detect the strokes during the inspiration that can not be palpable in the . It results from an accentuated decrease in blood pressure, which leads to the (radial) pulse that is not palpable and can be accompanied by an increase in height (). As is usual with inspiration, the increase is mild, due to the decrease in the left ventricular output. ContentMechanism[]During inspiration, negative intratoric pressure results in a right upper venous return, filling the right atrium more than during exhalation. The increase in the volume of blood spreads the right atrium, reducing the performance of the left atrium due to its shared sept. The lower left atrial performance reduces the venous performance of the left atrium and, as a result, causes a reduction in the left ventricular preload. This leads to a reduction in the volume of left ventricular stroke, and will be seen as a reduction in systolic blood pressure in inspiration. Therefore, the Pulsus paradox is an exaggeration or an increase in the fall of systolic BP beyond 10 mmHg during inspiration. [] Normally during inspiration, a person's systolic blood pressure decreases in ≤10 and the heart rate increases slightly. This is because inspiration decreases in relation to atmospheric pressure, which increases blood flow (systemic venous return) to the right atrium of the heart by reducing pressure on the veins, especially the vena cava. However, the decrease in intrathoracic pressure and the stretching of the lungs during inhalation also increases the compatible lung vasculature so that the blood ponds in the lungs and decreases the pulmonary venous return to the left atrium. In addition, the growing windy systemic return on the right side of the heart expands the right heart and directly compromises the filling on the left side of the heart by slightly hitting the sept on the left, reducing the maximum volume. The reduced left-heart filling leads to a reduced stroke volume that manifests as a decrease in systolic blood pressure, leading to a faster heart rate due to inhibition of the , which stimulates the heart. [] Under normal physiological conditions, the large pressure gradient between the right and left ventricles prevents the septol to lump dramatically into the left ventricle during inspiration. However, such lumping occurs during the heart tamponate where the pressure equals all the chambers of the heart. As the right ventricle receives more volume, it pushes the sept to the left ventricle further reducing its volume in turn. This additional loss of the volume of the left ventricle that only occurs with the equalization of pressures (such as in tamponade) allows the additional volume reduction, so the heart output is reduced, leading to an additional decrease in the PB. However, in situations where left ventricular pressure is still greater than the pericardial sac (most often of the co-existing disease with elevated left ventricular diastolic pressure), there is no pulsus paradox. Although one or both mechanisms can occur, one third can also contribute. The large negative intrathoracic pressure increases the pressure through the left ventricle wall (augmented transmural pressure, equivalent to [pressure inside the ventricle] - [pressure outside the ventricle]). This pressure gradient, resisting the contraction of the left ventricle, causes an increase in . This results in a decrease in , contributing to the decrease and increase of the heart rate as described above. [] Pulse paradoxus not only occurs with severe heart tamponate, but also with asthma, obstructive sleep apnea and breeding. The mechanism, at least with severe tamponada, is probably very similar to those of hypertrophic and restrictive cardiomyopathies ( diastolic dysfunction), where a decrease in the left ventricle filling (LV) corresponds to an ever smaller volume of traction. In other words, with these cardiomyopathies, as the LV filling decreases, the ejection fraction decreases directly, but not linearly and with a negative concavity (first and second negative derivation). Similarly, with tamponade, the degree of diastolic dysfunction is inversely proportional to the final-diastolic volume LV. So during inspiration, as the LV filling is less in relation to that during expiration, diastolic dysfunction is also proportionally greater, so systolic pressure falls Â10 mmHg. This mechanism is also likely with pericarditis, where diastolic function is punished. [] Measurement[ The pressure of the body (PP) is quantified by a stethoscope and (), measuring the variation of systolic pressure during expiration and inspiration. [] systolic To measure the paradox of the pulsus, place a fist of blood pressure on the patient's arm and deflate the fist very slowly while listening to the brachyal pulsations. Note the pressure you first hear with pulses during expiration (which will be the highest). Repeat the process and record the pressure of the clicks heard during the inspiration (which will be the lowest). [] If the pressure difference between the two readings is √10mm Hg, it can be classified as pulsus paradoxus. [] Causes[]Pulsus paradoxus can be caused by several physiological mechanisms. Anatomical, these can be grouped into: Considered physiologically, PP is caused by:[] List of causes[]Cardiac: Pulmonary: Non-pulmonary and non-cardiac: PP has proven to be predictive of the severity of the heart tamponada. Pulse paradox cannot be seen with cardiac tamponada if one or significant is also present. ######################### ################################################################################################################################################################################################################################# Other Other Other Other Other Navigation menu Personal tools Named spaces Variants Views More Search Navigation Contributed Tools Printing/exporting Other projects Languages
Pulsus paradoxus | European Respiratory Society
Plethysmograph Estimate of Pulsus Paradoxus Calculation . 1) AUC is... | Download Scientific Diagram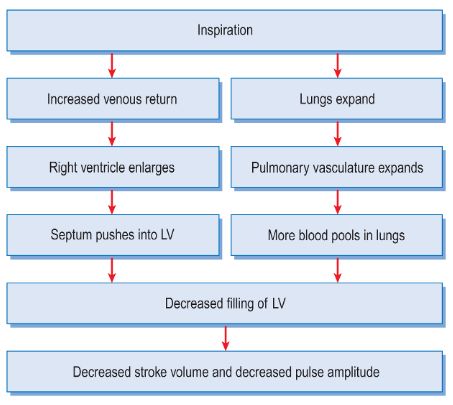
Pulsus Paradoxus - Clinical Examination | Epomedicine
Pulsus paradoxus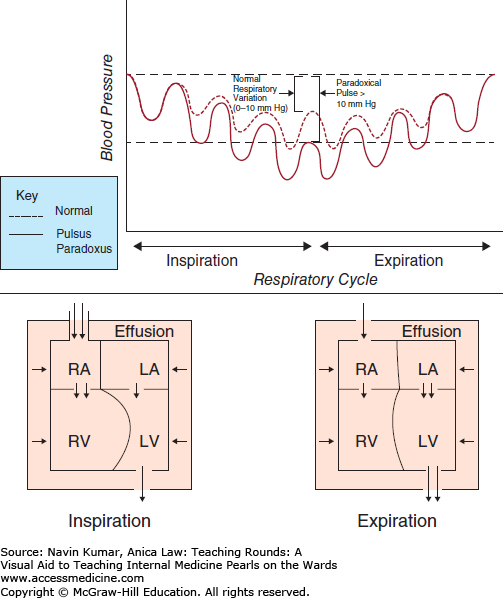
What is Pulsus Paradoxus? | Medicine Specifics
pulsus paradoxus | Cardiology nursing, Medical mnemonics, Icu nursing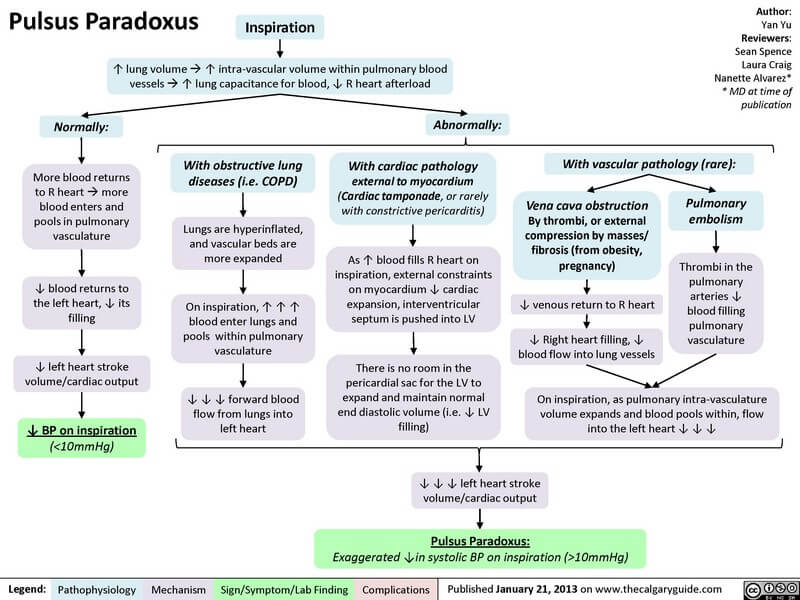
Pulsus Paradoxus - Clinical Examination | Epomedicine
Pulsus paradoxus | European Respiratory Society
Measurement and Mechanism of Pulsus Paradoxus | Download Scientific Diagram
Pulsus paradoxus | Cardiac auscultation, Cardiac, Nursing school
Cardiac tamponade | Deranged Physiology
Reversed Pulsus Paradoxus | NEJM
Classic Physical Sign Explained: Pulsus Paradoxus – MedicoWiki
Medical-Online - Pulsus paradoxus (PP), also paradoxic... | Facebook![Jack Penner on Twitter:]()
Jack Penner on Twitter: "[Take Homes] [1] Pulsus Paradoxus is not paradoxical [2] It is an EXAGGERATED fall in BP w/ inspiration due to - Decreased RV free wall expansion - Increased
Cardiac Tamponade- Pulsus Paradoxus - YouTube
Factors Influencing Pulsus Paradoxus in Asthma - CHEST
Pulsus Paradoxus - YouTube
Measurement and Mechanism of Pulsus Paradoxus | Download Scientific Diagram
Facebook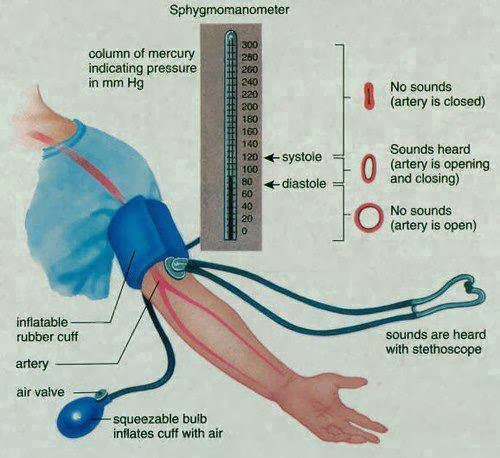
Pulsus Paradoxus- Correct technique of measurement - MedchromeTube
Pulsus alternans - Wikipedia
Reversed Pulsus Paradoxus | NEJM
Cardiac tamponade | Deranged Physiology
Chapter 19- Pathophysiology Flashcards | Quizlet![Anne Arnason on Twitter:]() 10 mm Hg of systolic blood pressure, or disappearance of radial pulse, during inspiration. [Though acc. to some" class="img-fluid" src="https://pbs.twimg.com/media/EhcM9vbXYAEgIzG.jpg" title ="Anne Arnason on Twitter: "3/ Regardless, Pulsus Paradoxus is defined by a decrease in >10 mm Hg of systolic blood pressure, or disappearance of radial pulse, during inspiration. [Though acc. to some"width ="100%" onerror="this.onerror=null;this.src='https://encrypted-tbn0.gstatic.com/images?q=tbn:ANd9GcRmm7q1krg60alJ7vUHd5rqVXfoFcb7o-PIPzDSmN5KwdbglzYniw';">
10 mm Hg of systolic blood pressure, or disappearance of radial pulse, during inspiration. [Though acc. to some" class="img-fluid" src="https://pbs.twimg.com/media/EhcM9vbXYAEgIzG.jpg" title ="Anne Arnason on Twitter: "3/ Regardless, Pulsus Paradoxus is defined by a decrease in >10 mm Hg of systolic blood pressure, or disappearance of radial pulse, during inspiration. [Though acc. to some"width ="100%" onerror="this.onerror=null;this.src='https://encrypted-tbn0.gstatic.com/images?q=tbn:ANd9GcRmm7q1krg60alJ7vUHd5rqVXfoFcb7o-PIPzDSmN5KwdbglzYniw';">
Anne Arnason on Twitter: "3/ Regardless, Pulsus Paradoxus is defined by a decrease in >10 mm Hg of systolic blood pressure, or disappearance of radial pulse, during inspiration. [Though acc. to some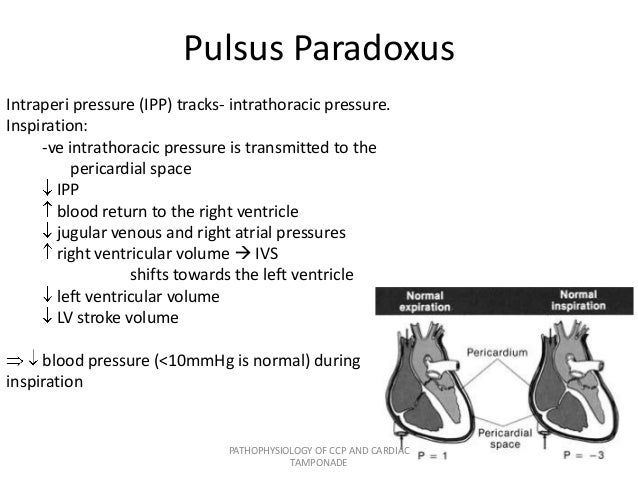
Pathophysiology of ccp and cardiac tamponade
pulsus paradoxus | Dr.S.Venkatesan MD
Oximetry-detected pulsus paradoxus predicts for severity in paediatric asthma | Archives of Disease in Childhood
Pulsus paradoxus | Med surg nursing, Nurse life, Chronic obstructive pulmonary disease
Pulsus Paradoxus: Cardiovascular Function and Assessment | EMS 12 Lead
ECG Case #19 - Question #2 Answer | LearntheHeart.com
Detection of Pulsus Paradoxus by Pulse Oximetry in Pediatric Patients After Cardiac Surgery | Semantic Scholar
Comparison between pulsus paradoxus and reversed pulsus paradoxus. | Download Table
Mechanism of reverse pulsus paradoxus - depends on etiology
Arterial pulse-variations - YouTube
JCI - Pulsus paradoxus.
Pulse rate and contour | medicalrojak
Pulsus paradoxus
Pulsus paradoxus - Sarkar - 2018 - The Clinical Respiratory Journal - Wiley Online Library
:max_bytes(150000):strip_icc()/pulsus-paradoxus-4587588-v1-593d02d7f4ab4380894939e7ce04c44d.png) Understanding the Mechanism of Pulsus Paradoxus
Understanding the Mechanism of Pulsus Paradoxus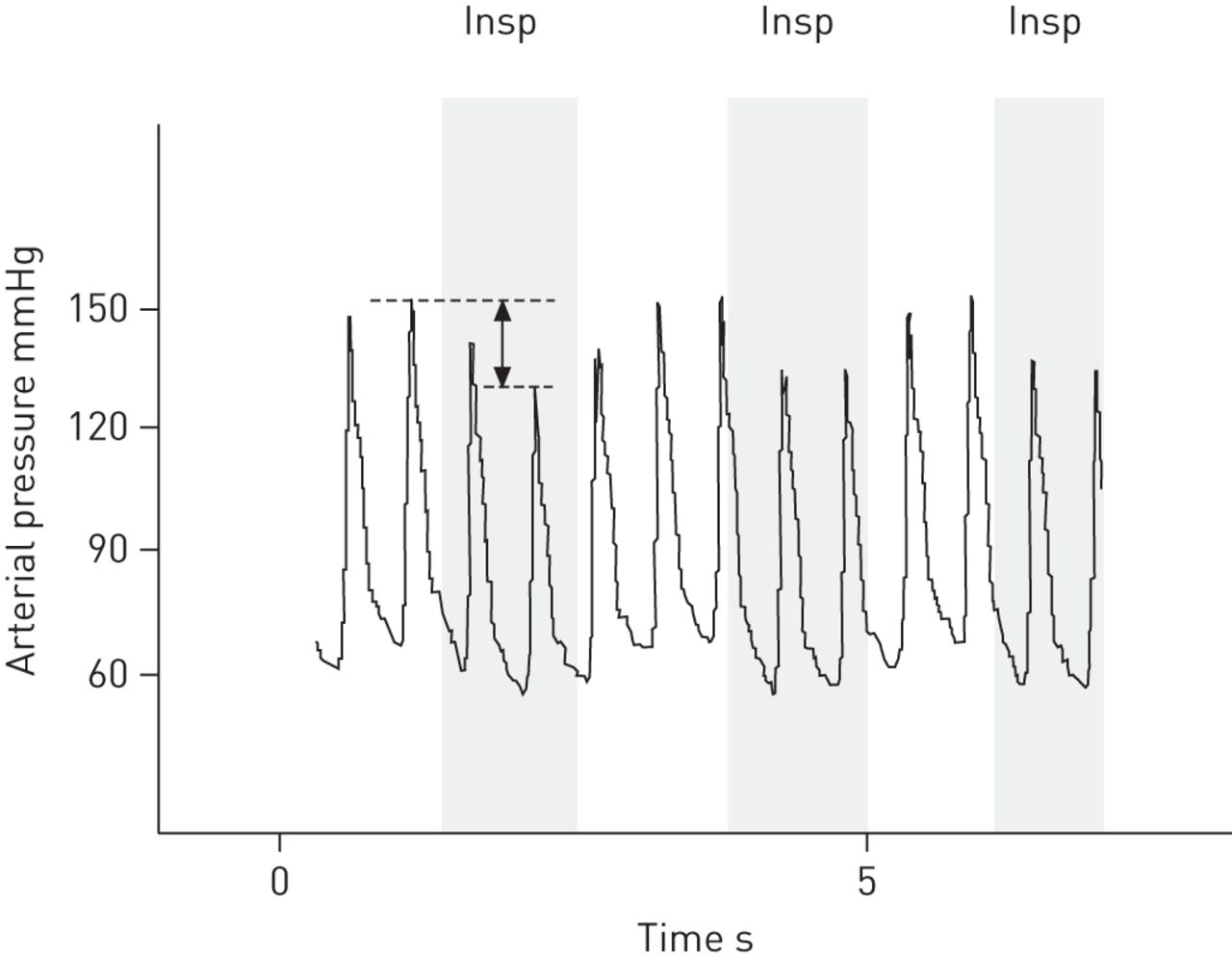




























Posting Komentar untuk "what is pulsus paradoxus"